Journal of Innate Immunity (2021)
Xinyu Zhuang, Günther Schlunck, Julian Wolf, Dennis-Dominik Rosmus, Tim Bleul, Ren Luo, Daniel Böhringer, Peter Wieghofer, Clemens Lange, Thomas Reinhard, Thabo Lapp
Number of citations (crossref.org): Loading....
Purpose: The pattern of immune cells infiltrating the corneal stroma has
been extensively studied in mice, but data on human tissue have been far less elaborate.
To further characterize the number and differentiation state of resident immune cells in organ-cultured human corneal
tissue, we employed a comprehensive bioinformatic deconvolution (xCell) of bulk RNA-sequencing (RNA-seq) data,
immunohistochemistry (IHC), and flow cytometry (FC).
Methods: A transcriptome-based analysis of immune cell types in human corneal
samples was performed. The results were validated by IHC, focusing on the identification of pro-inflammatory
(M1) and regulatory (M2) macrophages. A protocol was established to identify these 2 different macrophage
populations in human corneal tissue by means of FC. Subsequently, corneal samples in organ culture were
differentially stimulated by IL-10, IL-4 & IL-13, or LPS and macrophage populations were evaluated
regarding their response to these stimuli. Furthermore, cell survival was analyzed in
correlation with time in organ culture.
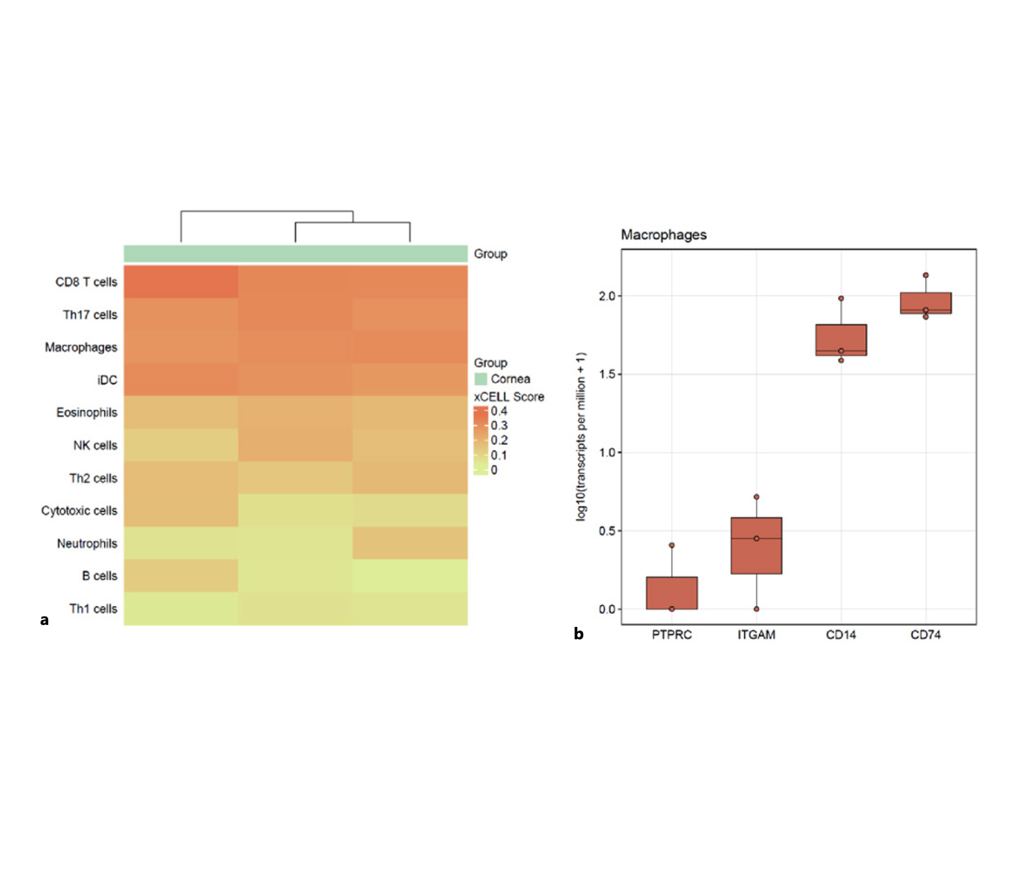
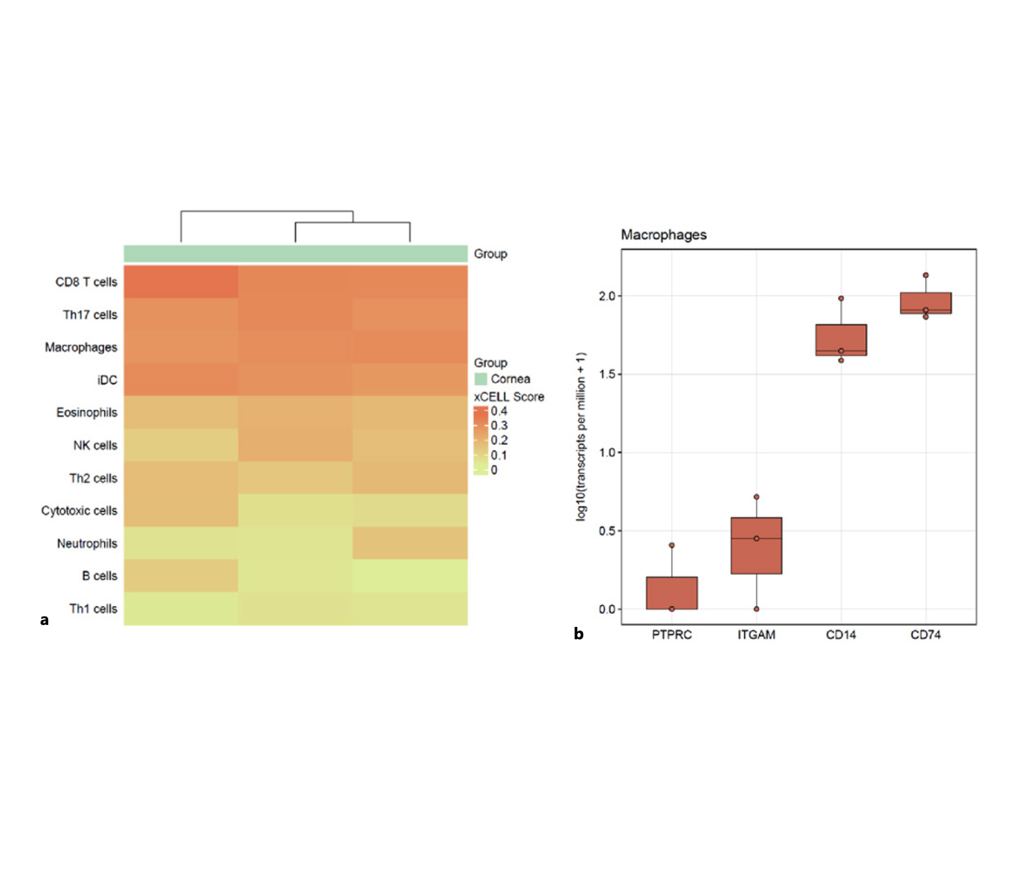
Results: xCell-based mathematical deconvolution of bulk RNA-seq data revealed the
presence of CD8 T cells, Th17 cells, dendritic cells, and macrophages as the predominant immune cell
types in organ-cultured human corneal tissue. Furthermore, RNA-seq allowed the detection of different
macrophage marker genes in corneal samples, including PTPRC (CD45), ITGAM (CD11b), CD14, and CD74.
Our RNA-seq data showed no evidence of a relevant presence of monocytes in human corneal tissue.
The presence of different macrophage subtypes was confirmed by IHC. The disintegration and subsequent
FC analysis of human corneal samples showed the presence of both M1 (HLA-DR+, CD282+, CD86+, and CD284+)
and M2 (CD163+ and CD206+) macrophage subtypes. Furthermore, we found that the total number of macrophages
in corneal samples decreased more than the total cell count with increasing tissue culture time. Treatment
with IL-10 led to higher total cell counts per cornea and to an increased expression of the M2 marker CD163 (p < 0.05)
while expression levels of various M1 macrophage markers were not significantly reduced by interleukin treatment.
Conclusions: Regarding different macrophage populations, untreated human corneas
showed more M1 than M2 macrophages. With increasing organ culture time, these macrophages decreased.
In terms of cell dynamics, adding interleukins to the organ culture medium influenced the phenotype of
macrophages within the cornea as detected by FC. Modifying the immunomodulatory properties of human grafts
appears a promising approach to further reduce the risk of graft rejection in patients. In this context,
treatment with interleukins was more effective in upregulating M2 macrophages than in suppressing M1
macrophages in corneal tissue.